The COVID pandemic has had immeasurable impacts on the lives of millions through illness, disability, and death. It has also dramatically shaped the work of asthma stakeholders. Asthma home visitors demonstrated remarkable adaptability by shifting to virtual visits, in part or in full. Clinicians have tried to make sense of the unexpected dip in asthma ED visits during the first year of the pandemic. Healthy housing advocates rose to the new challenge of rent debt and successfully advocated for eviction moratoria. Schools have made HVAC improvements, recognizing the important connection between indoor air quality and health. Above all, we have seen asthma stakeholders double down on our shared commitment to equity by prioritizing those communities unjustly burdened by both asthma and COVID.
As we at RAMP continue to work toward our mission during the pandemic, click here to learn what we’re doing to help keep communities healthy.
At RAMP, we have been tracking the literature on COVID-19 and asthma since the beginning of the pandemic. Read on for summaries of emerging research.
We also want to share what we’re learning about the implications of COVID-19 on people with asthma. Below is some summary information, supplemented by emerging research. We’ll update this webpage regularly.
COVID-19 and asthma
While early in the pandemic many feared that people with asthma would be at greater risk, a growing body of research suggests that people with asthma are neither more likely to contract COVID nor at greater risk of severe outcomes from COVID.
Researchers continue to explore whether asthma severity and/or phenotype impact COVID outcomes. The American Academy of Allergy, Asthma and Immunology notes, “Although the Centers for Disease Control and Prevention states that patients with moderate-severe asthma could be at greater risk for more severe disease, there are no published data to support this determination at this time. There have been many studies looking at the relationship between COVID-19 and asthma. Thus far the vast majority of these studies have found no increased risk of COVID-19 disease severity in those with asthma.” Regarding phenotype, a few studies have suggested that non-allergic asthma may be associated with more severe COVID-19 disease. However, there were limitations to those studies and experts agree that more research is needed on this topic. (For a helpful overview of asthma phenotypes, click here.)
Researchers also continue to explore whether asthma medications impact COVID outcomes. While chronic use of oral corticosteroids may increase the risk of COVID severity, research suggests that neither inhaled corticosteroids nor biologics increase risk. Some studies have suggested a beneficial effect of inhaled corticosteroids, but the majority of research studies show neither a positive nor negative impact and more research is needed.
Clinicians, researchers and public health experts agree that people with asthma should focus on keeping their asthma well controlled through following medication regimens and avoiding or reducing exposure to environmental asthma triggers.Keeping asthma well-controlled may be particularly important with regard to COVID as one study suggested people with well-controlled asthma have less severe COVID-19 outcomes than people with poorly-controlled asthma.
For additional information about COVID-19 and asthma, we recommend the following websites:
- American Academy of Allergy, Asthma and Immunology
- U.S. Centers for Disease Control and Prevention
- American Lung Association
- Asthma and Allergy Network
- Allergy and Asthma Foundation of America
COVID-19’s inequitable impacts
COVID has exacerbated many inequities that lead to disparate asthma outcomes. In California — like the rest of the nation – COVID disproportionately impacts low-income communities and communities of color. As just a few examples: the death rate for Latino people is 13% higher than the statewide rate and for Black people, it’s 18% higher. The case rate for Pacific Islanders is 79% higher than the statewide rate. The case rate for communities with median income of less than $40K is 23% higher than the statewide average (https://covid19.ca.gov/). These disparities are strikingly similar to asthma disparities, where low-income communities and communities of color often have a higher burden of asthma.
Social inequities contribute to COVID disparities. What do we mean by that? The California Department of Public Health explains, “Californians in crowded housing or transportation, and with less access to paid leave and other worker protections, have a higher risk of infection of COVID-19. Social determinants of health, such as food insecurity, lack of health insurance, and housing instability can increase the risk of poor outcomes. These social determinants of health are often the result of structural racism.” Research throughout the pandemic consistently shows that ongoing exposure to air pollution leads to worse COVID outcomes (for examples, click here). As a result of structural racism, sources of air pollution are disproportionately placed in low-income communities and communities of color.
COVID also exacerbates social inequities. Just a few examples include: People in low-income jobs were hit hardest by the pandemic. Many lost jobs or had hours reduced. School closures and childcare shortages had the greatest impact on the work of low-income women. Despite eviction moratoria that kept many people housed, rent debt has grown to the billions in California.
What does all this mean for our work to reduce the burden of asthma? We know that social inequities contribute significantly to asthma disparities (see RAMP’s Framework). COVID’s exacerbation of social inequities could lead to worsening health disparities, including asthma disparities. As a result, we are ever more committed to our mission of reducing the burden of asthma with a focus on equity. To that end, in 2022 RAMP adopted a new 3-year strategic plan that does just that. Read more here about our goals on Stable and Healthy Housing; Healthy Air for All; and Health Care Equity.
Emerging research
Posted April 23, 2024
Researchers Find No Link Between COVID-19 Virus and Development of Asthma in Children
In an article published in the journal, Pediatrics, on April 12, 2024, researchers from Children’s Hospital of Philadelphia share the findings of their retrospective cohort study of 27,423 children who had tested positive for COVID. They concluded that COVID is not associated with new asthma diagnosis in children. At the same time, their research confirmed that already known risk factors for pediatric asthma —Black race, food allergies, and allergic rhinitis– were indeed associated with new asthma diagnosis in children. Additionally, preterm birth and BMI were associated with new asthma diagnosis in children under 5 years old. Since the study focused solely on pediatric patients, not adult patients, more research will be needed to assess patients at different ages and at longer intervals to further confirm there is no relationship between COVID and the development of asthma overall.
COVID-19 and Asthma: What Have We Learned?
Posted May 8, 2023
In May 2023, an article by Dr. Chloe I Bloom with the National Heart and Lung Institute in London addressed Covid-19 pandemic and asthma: What did we learn? The review addresses some of the major lessons regarding asthma and the pandemic, and concludes the following:

Below is a brief explanation of each conclusion:
- Asthma control and adverse COVID outcomes: The author shared that, since the beginning of COVID, a huge number of studies have been published trying to answer the question of whether asthma is associated with worse COVID-19 outcomes. She shares a table of key studies and concludes, “Put together, these findings suggest that poor asthma control, not asthma severity, is a risk factor for worse covid-19 outcomes.”
- Inhaled corticosteroids and COVID: The author notes that a popular theory has been that inhaled corticosteroids have a protective effective against severe COVID outcomes and reviews studies that have explored this question. She concludes that if inhaled corticosteroids have a protective effect against severe COVID outcomes, it is likely because they help individuals get their asthma well controlled, linking back to her first conclusion on the importance of asthma control.
- COVID vaccines and asthma: The author reviewed studies showing that COVID-19 vaccines are safe for people with asthma and noted “The most important message here is the importance of vaccinations for asthma patients, not just against covid-19, but also to prevent influenza and pneumonia.”
- Public health prevention and asthma exacerbations: The article also included a discussion of potential reasons for the initial significant drop in hospital admissions for asthma. Ms. Bloom described that the most compelling evidence suggests that this is due to “a sustained change in exposure to respiratory viruses.” She reviewed evidence from different countries showing that asthma hospitalizations decreased when there were stringent public health prevention measures in place. When the measures became less stringent, there was a rise in respiratory viruses like rhinovirus, and a rise in asthma exacerbations.
- Telemedicine and asthma: There was a rise in telemedicine during the pandemic and the author notes many articles citing the benefits of telemedicine for asthma management, yet also acknowledges some challenges related to equity. She concludes, “A combination approach of both in-person visits and telemedicine may be the optimal clinical practice to maximize patient experience and increase healthcare access and minimize health disparities.”
- Long COVID and asthma: Lastly, the author concluded that people with asthma experience more lung-related symptoms post-COVID but that we need more studies to explore whether there is also an increased risk of other long COVID aftereffects.
Study Shows Increase in Healthcare Utilization for Asthma Among Adults with Long COVID
Posted March 17, 2023
In an article published earlier this month in the Journal of the American Medical Association, researchers shared results of a case-control study (of 13,435 US adults with long COVID and 26,870 matched adults without COVID-19) that looked at rates of adverse health events over the 12-month follow-up period. Even after accounting for risk factors present pre–COVID-19, adults with long COVID had increased rates of cardiovascular and pulmonary outcomes, and the increase was more pronounced for adults that had been hospitalized for COVID. In the 12 months following infection, adults with long COVID saw an increase of 24.2% in healthcare utilization for asthma, compared to 12.4% in the control group. That’s a relative risk of 1.95 (95% CI, 1.86-2.03). The increase of healthcare utilization for asthma among adults with long COVID who had been hospitalized for COVID was 31.6% compared to 14.7% for the control group, which is an increase in relative risk of 2.15 (95% CI, 2.00-2.31). The authors note, “These findings will improve understanding of care needed for individuals with [long COVID], as well as inform health care systems directing resources toward surveillance, follow-up, and case management to this population.”
AAAAI Issues Guidance on Pulmonary Office Procedures During the COVID-19 Pandemic
Posted September 21, 2022
The COVID-19 pandemic has placed increased demands on the ability to safely perform pulmonary procedures that are critical to asthma management. Accordingly, the American Academy of Allergy, Asthma & Immunology (AAAAI) Asthma Diagnosis and Treatment convened a work group to offer guidance. The work group is composed of specialist practitioners from academic and both large and small practices. Individuals with special expertise were assigned sections on spirometry, fractional exhaled nitric oxide, nebulized treatments, and methacholine challenge. Their guidance can be found here in the Journal of Allergy and Clinical Immunology. They consider relative risk of each procedure, depending on the environment of care, community transmission rates, and the individual patient’s risk factors. They also recommend a number of strategies for reducing the risk of COVID transmission while still performing important pulmonary procedures.
Study Shows Connection Between Air Pollution and Increased Risk for COVID Infection and Death in CA
Posted August 15, 2022
California is home to some of the highest concentrations of air pollution in the nation. A study released in August, 2022, by the Public Health Institute’s Tracking California program reveals that air pollution increases the risk of COVID-19 infection and death. The study, Association Between Long-Term Exposure to Particulate Air Pollution with SARS-CoV-2 Infections and COVID-19 deaths in California, U.S.A, was conducted in partnership with researchers from the University of California, San Francisco. It’s set to be published in the October, 2022, edition of Environmental Advances.
Previous studies have reported a connection between air pollution and COVID-19 morbidity and mortality and have focused their exposure assessment on areas larger than local neighborhoods. This is the first study of its kind for California that looks at neighborhood-level air pollution data and examines over 3 million SARS-CoV-2 infections and about 50,000 COVID-19 deaths in California from February 2020 to February 2021 to evaluate the risks associated with long-term levels of fine particulate matter (PM2.5). High levels of the air pollutant PM2.5 can negatively impact our health and can cause asthma, lung cancer and other respiratory diseases. The study also focuses on individual-level data, such as age and gender.
When compared to those living in neighborhoods with the lowest PM2.5 exposure, researchers found that individuals living in neighborhoods with the highest long-term PM2.5 exposure were:
- At 20% higher risk of SARS-CoV-2 infections
- At 51% higher risk of COVID-19 mortality
- More likely to be Hispanic and from low-income communities
Areas with the greatest concentration of PM2.5 were California’s San Joaquin Valley and South Coast air basins. Researchers estimate that 9% or approximately 4,250 COVID-19 deaths during the study period could have been prevented if the entire state met the National Ambient Air Quality Standards for PM2.5. The standards include the maximum allowable levels for the fine particulate matter analyzed in this study, a pollutant which is of high public health concern, as it can be inhaled deeply into the lungs.
To see the study’s abstract, click here. The full study is here. For a program overview, click here.
Impact of the pandemic on asthma control in African American children
Posted July 14, 2022
In June 2022, researchers based on Brookdale Hospital Medical Center in New York published in Cureus the results of a study on the impact of COVID-19 on asthma control. The retrospective, pre-post, comparative cross-sectional study of 104 majority African American pediatric patients with asthma before and after the changes caused by COVID-19 shows that there were significant improvements in asthma outcomes after COVID-19 societal changes when compared to before COVID-19 based on primary medical doctor visits, ED visits, hospitalizations, pediatric intensive care unit admissions, and courses of systemic steroids for asthma exacerbations. These findings are consistent with similar studies performed on other populations of asthma patients, but this study is noteworthy for its focus on African American children who are both disproportionately impacted by asthma and underrepresented in research studies.
The researchers also sought to investigate the use of telemedicine among participants, which could provide additional tools for providing healthcare to an underserved population. Telemedicine visits increased during the pandemic and the asthma outcomes suggest that they may be equal to or better than in-person visits. Researchers note that “follow-up studies on the effects of telemedicine pulmonology care on asthma outcomes compared to in-person visits, barriers to telemedicine usage among the African American population, and studies on the rates of telemedicine usage among African Americans compared to in-person visits, may help provide valuable new tools for clinicians and patients and reduce the barriers to medical care among patients that are impacted by systemic inequities and inequalities.”
Telemedicine in asthma management during COVID
Posted June 2, 2022
In May, 2022, researchers published a review in Current Treatment Options in Allergy about how COVID has shaped the evaluation and management of asthma. The authors explain, “The comprehensive management of asthma has historically relied on in-person visits to obtain a detailed history, thorough physical exam, and diagnostic and monitoring tools such as pulmonary function testing. The COVID-19 pandemic has posed numerous challenges to adequately utilizing these strategies. Despite these limitations, telemedicine has provided an important means to deliver asthma care. In this review, we discuss how these challenges have created paradigm shifts in not only the clinical aspects of asthma management, but also in patient attitudes and physician-patient relationships.”
Asthma as a predictor of Long COVID
Posted June 2, 2022
In a January, 2022, article in Nature Communications, researchers looked at risk factors for post-acute COVID syndrome, or Long COVID. In a prospective multicentric cohort study of 215 individuals, they studied COVID-19 patients during primary infection and up to one year later, compared to healthy subjects. Researchers observed an association of risk of developing long COVID with a history of lung disease (odds ratio 6.29; p = 0.004) and, particularly, asthma (odds ratio 9.74; p = 0.003). While the study has limitations, including a small sample size, it provides an important observation as the field works to increase our understanding of Long COVID.
A review of asthma and COVID
Posted June 2, 2022
In December, 2021, researchers in Israel published an update on asthma and COVID in European Respiratory Review. They concluded that asthma is not an independent risk factor for infection or disease severity. They explain: “Furthermore, asthma is not over-represented in hospitalised patients with severe pneumonia due to SARS-CoV-2 infection and there was no increased risk of asthma exacerbations triggered by SARS-CoV-2.” The authors note that phenotype, severity, and comorbidities may be important factors in evaluating the risk of COVID infection and outcomes; however, more research is needed. They also looked at the research on different asthma medications as they relate to COVID outcomes. Data indicate the use of inhaled corticosteroids (ICS) is safe in asthma patients with COVID . Furthermore, “it has been proposed that ICS may confer some degree of protection against SARS-CoV-2 infection and the development of severe disease by reducing the expression of angiotensin converting enzyme-2 and transmembrane protease serine in the lung…. Most of the epidemiological studies have reported that there is no evidence that the use of ICS either increases SARS-CoV-2 infectivity and COVID-19 severity or has a beneficial effect on outcome.” The authors explain, however, that chronic or recurrent use of systemic corticosteroids before COVID infection is a major risk factor of poor outcomes in asthma patients. In contrast, research suggests that biologics are safe. Below is a summary table of the authors’ conclusions about asthma medications.

Safe Cleaning Tips and Resources During the COVID Pandemic
Posted June 1, 2021
Early in the pandemic, there was a lot of concern about fomite (surface) transmission. However, as our knowledge about COVID has grown, concern about the risk of transmission from touching surfaces has reduced. Per the CDC: “The virus that causes COVID-19 can land on surfaces. It’s possible for people to become infected if they touch those surfaces and then touch their nose, mouth, or eyes. In most situations, the risk of infection from touching a surface is low.”
Recently the Centers for Disease Control and Prevention (CDC) updated its guidance for when to clean and when to disinfect in non-healthcare facilities. The new guidance emphasizes that when no people with confirmed or suspected COVID-19 are known to have been in an indoor setting within the last 24 hours, cleaning once a day is enough to keep a facility healthy.
The Occupational Health Branch (OHB) of the California Department of Public Health shared a reminder that “When following this or any cleaning and disinfecting guidance it is important to know that disinfectants and cleaners often contain chemicals that can cause or trigger asthma.” They shared the following tips and resources.
Tips
- As indicated in the guidance, disinfect only when necessary. Routine cleaning performed effectively with soap or detergent can substantially reduce virus and bacteria levels on indoor surfaces.
- The U.S. Environmental Protection Agency (EPA) created a list of disinfectants that work to kill coronavirus. Choose hydrogen peroxide (without peracetic acid), lactic acid, citric acid, silver, or alcohol-based products whenever possible. These are not known to cause asthma.
- Use as much ventilation as possible. Open windows if needed.
- Dilute products properly. Do not make them more concentrated than the labels say.
- Follow recommendations on the label or the safety data sheet. This may include wearing gloves or goggles.
- Choose fragrance-free cleaning products.
Resources
- Work-Related Asthma, Cleaning Products, and Disinfectants – OHB web page
- Reminders for Using Disinfectants at Schools and Child Cares (PDF) | Spanish – California Department of Pesticide Regulation InfoSheet
- Fragrances and Work-Related Asthma – OHB web page
- Cleaning for Asthma-Safe Schools (CLASS) – OHB web page
- Work-Related Asthma Prevention Program (WRAPP) – OHB website
The Role of Airborne Transmission of COVID-19 and Mitigation Measures
Posted May 3, 2021
Back in October, 2020, we shared a link to a document of FAQs on Protecting Yourself from COVID-19 Aerosol Transmission, developed collaboratively by scientists and engineers with many years of collective research experience related to indoor air quality, aerosol science, aerosol disease transmission, and engineered control systems for aerosols. While the authors continue to update the document as research evolves, new research has also been published to further detail the role of aerosol transmission in the COVID-19 pandemic. On May 2, 2021, a pre-print publication was released on “Indicators for Risk of Airborne Transmission in Shared Indoor Environments and their application to COVID-19 Outbreaks”. The authors propose two simple parameters as indicators of infection risk for indoor environments. They combine “the key factors that control airborne disease transmission indoors: virus-containing aerosol generation rate, breathing flow rate, masking and its quality, ventilation and air cleaning rates, number of occupants, and duration of exposure. COVID-19 outbreaks show a clear trend in relation to these parameters that is consistent with an airborne infection model, supporting the importance of airborne transmission for these outbreaks.” Their analysis shows that mitigation measures are needed to limit aerosol transmission risk in most indoor spaces. Among effective measures are reducing vocalization, avoiding intense physical activities, shortening duration, reducing occupancy, wearing high-quality well-fitting masks, increasing ventilation and applying additional virus removal measures (e.g. using HEPA filters). The authors conclude that “The use of multiple ‘layers of protection’ is needed in many situations, while a single measure (e.g. masking) may not be able to reduce risk to low levels.” The use of HEPA filters and increasing ventilation can also benefit people with asthma, as they improve indoor air quality.
Posted April 26, 2021
As shared in RAMP’s previous updates on emerging research related to COVID-19 and asthma, multiple early reports of patients admitted to the hospital with COVID-19 showed that people with asthma and other chronic respiratory disease were significantly under-represented. Some researchers have suggested that asthma might provide some protection against severe COVID-19 outcomes. On April 9, 2021, in The Lancet Respiratory Medicine, researchers, “hypothesised that the widespread use of inhaled glucocorticoids among these patients was responsible for this finding, and tested if inhaled glucocorticoids would be an effective treatment for early COVID-19.” The researchers conducted a randomized controlled trial of inhaled budesonide (Pulmicort), compared with usual care, in adults within 7 days of the onset of mild COVID-19 symptoms. The findings were that inhaled budesonide “reduced the likelihood of requiring urgent care, emergency department consultation, or hospitalization. There was also a quicker resolution of fever, a known poor prognostic marker in COVID-19, and self-reported and questionnaire-reported symptom resolution was faster. There were fewer participants with persistent COVID-19 symptoms at days 14 and 28 after budesonide therapy compared with usual care.” While the authors noted some limitations in their study, the findings are exciting because budesonide is a low cost, safe, simple, and widely available therapeutic option around the world. They noted that future research should explore whether the effect they observed is exclusive to budesonide or represents a class effect of inhaled corticosteroids. For additional information, click here.
Admissions to US Hospitals Decreased in 2020 Across an Array of Pediatric Conditions, Including Asthma
Posted April 5, 2021
A recent study published in the Journal of the American Medical Association Network – Open looked at over 5 million admissions at 49 hospitals in the Pediatric Health Information Systems database, comparing 2020 data to prior years. The authors found a significant reduction (up to 45.4%) in admissions across numerous health issues. The following graph shows pediatric hospital admissions for asthma, by month. The gray, blue, and black lines show data from 2010-2019 and the red line shows data from the first half of 2020.
With regard to asthma, the authors note an overall reduction in respiratory infections, suggesting that human behavior (social distancing and masking) can reduce hospital admissions. They suggest that it could also be due to unmet care needs, noting “One inpatient survey suggested that greater than one-third of parents delayed seeking medical care for their child because of fears surrounding COVID-19.”
Posted March 23, 2021
Many states have entered the stage of COVID-19 vaccine distribution that prioritizes people with certain health conditions that put them at high risk for extreme complications from COVID-19. This has led many health care professionals serving patients with asthma to ask, “is asthma a risk factor for severe disease?”
The American Academy of Allergy Asthma & Immunology’s (AAAAI) COVID-19 Response Task Force wrote, “At this point, the answer is no.” Its members explain, “We all continue to get questions about asthma and COVID-19 from our patients. Earlier in the pandemic, they were concerned about getting sick and now they are concerned about which vaccine tier they should be in. By early October of this past year, there have been over 110 publications including 4 meta-analyses that clearly demonstrate that asthma is not a risk. Similar findings are noted in the 10 or so papers published since then, and at least a few have demonstrated protection for those with asthma.” (Click here for additional references.)
The Asthma and Allergy Foundation of America (AAFA) also affirms this with its statement: “Asthma is not a higher risk condition for COVID-19. Check your state’s COVID-19 vaccine plan to see when you might be eligible to receive the vaccine.”
Both AAAAI and AAFA will continue to update their websites as more information about vaccines that may be of interest to people with asthma and allergies. Meanwhile, the message from both organizations is clear: everyone should get a COVID-19 vaccine, but there is no reason that people with asthma should be prioritized based on current research.
U.S. EPA Shares Webinars and Tools on Addressing IAQ and COVID-19 in Schools
Posted March 8, 2021
The U.S. Environmental Protection Agency recently hosted a series of webinars on indoor air quality (IAQ) and schools throughout 2020, many of which focused specifically on how proper IAQ management also reduces COVID-19 risk. Specifically, through viewing the webinars, you can learn:
- strategies for operating and maintaining efficient HVAC systems to provide clean and healthy air in schools;
- how to tailor your cleaning and maintenance plans and procedures to help implement cleaning guidance for schools and reduce the spread of viruses and bacteria;
- strategies for developing a comprehensive IAQ management plan to proactively prevent the spread of viruses and bacteria in schools; and,
- strategies for reducing aerosol exposure.
On February 20th, the European Journal of Allergy and Clinical Immunology shared the results of a multinational cohort that included 1,054 children with asthma and 505 non-asthmatic children aged between 4-18 years from 25 pediatric departments, from 15 countries globally. Consistent with other recent research, the findings were that childhood asthma outcomes, including control, were improved during the first wave of the COVID‐19 pandemic, “probably because of reduced exposure to asthma triggers and increased treatment adherence.” The researchers concluded that “The decreased frequency of acute episodes does not support the notion that childhood asthma may be a risk factor for COVID‐19. Furthermore, the potential for improving childhood asthma outcomes through environmental control becomes apparent.”
Posted February 8, 2021
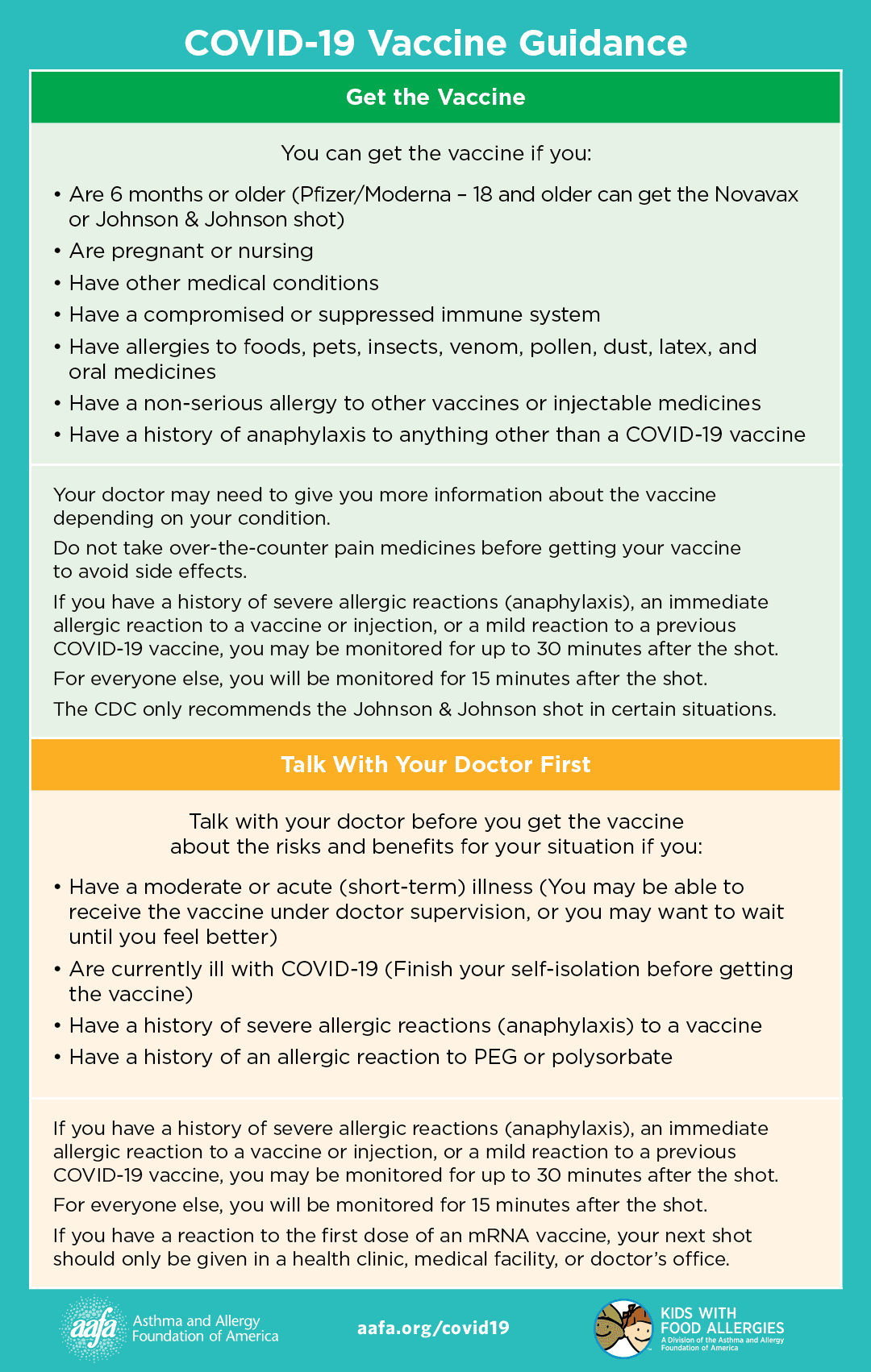
Given that many people with asthma also have allergies, providers may receive questions from patients with asthma about possible allergic reactions to COVID-19 vaccines. The American Academy of Allergy, Asthma and Immunology COVID-19 task force is providing updates on the recommendations and research. In short, at this point, the recommendations are as follows:
- All COVID-19 vaccines should be administered in a facility where each person can be monitored for at least 15 minutes with treatment readily available for anaphylaxis. Anyone with a history of non-anaphylactic reactions to food, oral medication, latex, environmental, or venom allergens can safely receive either the Pfizer or Moderna vaccine in this manner.
- Anyone with a history of anaphylaxis to food, oral medication, latex, environmental, or venom allergies can receive either the Pfizer or Moderna vaccine without any precautions other than a recommended 30-minute observation period.
- Anyone with a history of immediate onset hypersensitivity reactions (urticaria, wheezing, angioedema, anaphylaxis) to any prior vaccine or injected medication can receive either the Pfizer or Moderna vaccine with a recommended 30-minute observation period. Consultation with an allergist to discuss risks/benefits may also be considered.
- Anyone with known and proven IgE-mediated reactions to polyethylene glycol or polysorbate are currently advised to avoid the Pfizer and Moderna vaccines. Given the rarity of allergies to these ingredients, it is unlikely for anyone to have this known allergy, unless specifically evaluated by a board certified allergist and confirmed with prior skin testing.
Beating the Surge with Control of Airborne Exposure: Practical Tools to Prevent Airborne Virus Transmission Risk
Karen Cohn, MS, Certified Industrial Hygienist, Senior Public Health Consultant and former Program Manager, San Francisco Department of Public Health’s Children’s Environmental Health Promotion Program, just released a presentation on reducing airborne virus transmission risk. The slides can be found here and here. The presentation includes: what we know about airborne transmission of COVID-19; using ventilation and filtration to reduce airborne transmission; and the role of temperature, humidity, and other factors in COVID-19 transmission. The presentation includes scientific evidence, practical tips, and small group learning activities.

Declining Pediatric Emergency Department Visits for Asthma and COVID-19 Shut-downs
Researchers Simoneau et al from Boston Children’s Hospital just published in the Annals of the American Thoracic Society their research on the impact of COVID-19 on emergency department utilization for asthma. After adjusting for year, weeks and time period (pre- or post- shutdown), they found a significantly decreased incidence of ED visits after the COVID-19-related shut-down in 2020 compared to 2018 and 2019. While the reasons for this significant decrease are unclear, the authors suggest several potential contributors to this decrease, including “increased adherence to asthma medications, avoidance of the healthcare setting due to fear of contracting COVID-19, improved air quality due to work-from-home implementation, decreased participation in sports and exercise, decreased exposure to outdoor aero-allergens, and decreased viral exposure due to school/daycare closure. Interestingly, rather than a gradual decline, which would be more indicative of improved medication adherence, there was a dramatic decline, suggestive of a sudden change in exposure, which occurred in conjunction with the stay at home order and school closure.” The authors note that their research only looked at data for their own hospital and additional research is needed to assess whether this dynamic is similar elsewhere. They note that this could provide an important opportunity to identify factors that can be controlled in the future to improve asthma management.
The Impacts of the COVID-19 Pandemic on the Management of Asthma
Posted December 7, 2020
Most articles addressing asthma and COVID-19 have looked at the relationship between the likelihood of acquiring the illness and the likelihood of severe illness outcomes. Taking a different approach, an article published in the Journal of Allergy and Clinical Immunology Practicein September, authors Oreskovic et al look at how the COVID-19 pandemic impacts asthma management. The authors describe, “Sudden dramatic changes in the environment, medical practice, and medication use have altered the asthma management landscape with potential impacts on asthma outcomes.” They look at how changes in transportation and travel patterns, school attendance, physical activity, time spent indoors, and changes in health care delivery since the start of the pandemic play a role in asthma control in children. The figure below, included in the article, summarizes the impacts– both positive and negative– of these pandemic-driven factors on asthma control.

One Study Shows Asthma Associated with Decreased Risk of COVID-19 in Children
Posted November 16, 2020
The question of whether and how asthma and COVID-19 are related has been an ongoing question since the pandemic’s start. According to the American Academy of Asthma, Allergy, and Immunology, “Few data exist to indicate that having asthma is associated with an increased risk of becoming infected with COVID-19 or a more severe course. Recent reassuring data show that having asthma was not associated with an increased risk of hospitalization or even mortality in COVID-19 hospitalized patients.”
Wildfire Smoke Associated with Poorer COVID-19 Outcomes
Researchers published an article in the October edition of European Review of Medical and Pharmacological Sciences, looking at the impact of wildfire smoke on COVID-19 in San Francisco. The researchers looked at daily COVID-19 cases, deaths, particulate matter (PM-2.5 μm) and carbon monoxide from March 20, 2020 to Sept 16, 2020. They found that a one micrometer (μg/m3) increase in PM2.5 were associated with an increase in the daily COVID-19 cases, cumulative cases and cumulative deaths by 0.5%, 0.9% and 0.6%, respectively. Additionally, with a 1 part per million (ppm) increase in carbon monoxide level, the number of daily COVID-19 cases, cumulative cases and cumulative deaths increased by 5%, 9.3% and 5.3%, respectively. They concluded that, “The wildfire allied pollutants, particulate matter PM-2.5μm and CO have a positive association with an increased number of SARS-COV-2 daily cases, cumulative cases and cumulative deaths in San Francisco.”
Scientists Collaborate on FAQs To Protect Yourself from COVID-19 Aerosol Transmission
Posted October 19, 2020
Scientists and engineers with many years of collective research experience related to indoor air quality, aerosol science, aerosol disease transmission, and engineered control systems for aerosols have come together to produce a publicly accessible document on FAQs on Protecting Yourself from COVID-19 Aerosol Transmission. The authors explain, “The goal of these FAQs is to provide information to the general public in an efficient manner about how to prevent aerosol transmission of COVID-19, with the hope that this will allow more informed decision making by individuals or organizations… Having multiple experts working together, and having the ability to update this information also improves its quality.” The FAQs address such information is the definition of aerosol transmission, the distinction between aerosol and droplet transmission, the role of humidity and temperature on aerosol transmission, and the length of time that SARS-CoV-2 remains infectious in aerosols. This information is then followed up a robust list of recommendations, addressing such things as aerosol transmission in cars, schools, airplanes, and outdoors, as well as the role of masks, ventilation, and filtration in limited aerosol transmission. Click here to review the FAQs.
Inequitable Access to Telemedicine During the COVID-19 Pandemic
Research Shows Disproportionate Rate of Coronavirus Deaths in Polluted Areas
Posted September 21, 2020
COVID-19 can be made more serious by a specific type of industrial emission called hazardous air pollutants, or HAPs, according to peer-reviewed research by ProPublica and researchers at the State University of New York College of Environmental Science and Forestry, published on September 11, 2020 in Environmental Research Letters. Their focus on HAPs builds upon earlier studies linking poor air quality to COVID-19 mortality, which focused solely on criteria pollutants. This study examined the relationship between HAP exposure and COVID-19 mortality, while controlling for socioeconomic status, population health indicators, and exposure to PM2.5 and ozone. The researchers conclude, “We find that an increase in the respiratory hazard index is associated with a 9% increase in COVID-19 mortality. Although differing in magnitude, this association holds for individual HAPs acetaldehyde, and diesel PM [particulate matter]. These findings help us to understand variation in US-based COVID-19 mortality rates, reinforce existing research linking air pollution to mortality, and emphasize the importance of regulatory efforts to limit air pollution exposure risk.”
Posted September 14, 2020
On September 4, 2020, the American Association of Asthma, Allergy and Immunology (AAAAI) published a summary of research to date on asthma and COVID-19. In describing the article, the authors write, “There have been many studies looking at the relationship between COVID-19 and asthma. Thus far, the vast majority of these studies have found no increased risk of COVID-19 disease severity in those with asthma. Further, there appears to be no indication that asthma is a risk factor for developing COVID-19 disease. However, a few studies have suggested that non-allergic asthma may be associated with more severe COVID-19 disease, although it is not clear in these studies that subjects did not have COPD, which is a well-established risk for severe COVID-19. A few studies have also suggested a higher rate of intubation in asthma patients hospitalized with COVID-19, but other studies have not replicated these findings. Finally, early data from New York State had suggested a reduced death rate in asthma patients hospitalized with COVID-19, but this has not been reproduced in other studies. Taken together, it appears that there is either no risk or at most a very slight risk for more severe COVID-19 disease in non-allergic asthma patients. This is in contrast to other risk factors like COPD, obesity, etc., that have consistently been linked to more severe COVID-19 disease.” The full summary is available here.
While most California schools have begun the year with remote learning, many children have returned to school in other parts of the country. As school staff, parents and students grapple with the many considerations of returning to school during a pandemic, people with asthma may have additional considerations.
Fortunately, some great resources and guidance have already been developed. As we previously shared, in June, 2020, the Asthma and Allergy Foundation of America released COVID-19 and Asthma Toolkit for Schools designed to address the major challenges schools are facing in the 2020-2021 school year. School administrators, nurses and staff can use this toolkit to create an environment that can help protect students and staff with asthma, while preventing the spread of the new coronavirus.
As another resource, the most recent edition of The Lancet: Respiratory Medicine, on September 1, 2020, includes commentary on the topic. The authors discuss the importance of proactive asthma management and symptom monitoring, flu vaccines, and a focus on the social determinants of health impacting asthma, particularly given the economic impacts of the pandemic.
Additionally, the Center for Cities and Schools at the University of California Berkeley recently launched a clearinghouse of resources and tools developed by experts to assist local schools and states in safely and equitably reopening their school facilities.
Posted August 31, 2020
- It is important to reduce exposure to wildfire smoke by avoiding outdoor activities, whenever possible.
- Keep in mind that the cloth masks that are used to slow the spread of COVID-19 do not offer protection against wildfire smoke. Although N95 respirators do provide protection from wildfire smoke, they might be in short supply as frontline healthcare workers use them during the pandemic.
- Seeking clean air shelters and clean air spaces can help reduce exposure. However, given that social distancing guidelines are in place, finding cleaner air might be harder if public facilities such as libraries, community centers, and shopping malls are closed or have limited their capacity.
- If possible, create cleaner air spaces at home through:
- Using a portable air cleaner in one or more rooms. Portable air cleaners work best when run continuously with doors and windows closed.
- Create a do-it-yourself box fan filtration unit However, never leave it unattended.
- Whenever you can, use air conditioners, heat pumps, fans, and window shades to keep your cleaner air space comfortably cool on hot days.
- If you have a forced air system in your home, you may need to speak with a qualified heating, ventilation, and air conditioning (HVAC) professional about different filters (HEPA or MERV-13 or higher) and settings (“Recirculate” and “On” rather than “Auto”) you can use to reduce indoor smoke.
- Avoid activities that create more indoor and outdoor air pollution, such as frying foods, sweeping, vacuuming, and using gas-powered appliances.
- Know the difference between symptoms from smoke exposure and COVID-19
- Some symptoms, like dry cough, sore throat, and difficulty breathing can be caused by both wildfire smoke exposure and COVID-19.
- Learn about symptoms of COVID-19. Symptoms like fever or chills, muscle or body aches, and diarrhea are not related to smoke exposure.
- If you have severe symptoms, like difficulty breathing or chest pain, immediately call 911 or the nearest emergency facility.
Posted August 10, 2020
On August 4th, researchers from the National Health Service published an article in The Lancet: Respiratory Medicine on “COVID-19 and preschool wheeze care: lessons learned.” The authors explain that, “The pattern of increasing visits to the emergency department by children younger than 5 years with preschool wheeze and other respiratory conditions has been disrupted by the COVID-19 pandemic. Since March, 2020, presentations to the emergency department have decreased among children of all age groups, especially infants and preschool children who are the most frequent attenders. This notable change in asthma exacerbations in children has raised research interest into how the COVID-19 pandemic has contributed to this change, and what lessons can be learned.” The authors suggest several potential reasons for the decrease in emergency department visits. For example, they raise the possibility of a decrease in exposure to secondhand smoke. Although the data are inconclusive, the authors point to some data indicating that people have at least attempted smoking cessation during the pandemic. Another possible reason for the decrease in emergency department visits may be the increased use of effective telemedicine strategies. The publication includes recommendations to sustain and ramp up efforts to reduce exposure to environmental asthma triggers and to enhance effective telemedicine strategies. For more details, including other hypotheses, click here.
Study Suggests Type of Asthma (Allergic vs. Non-allergic) Impacts COVID-19 Severity in Adults
Posted August 3, 2020
Researchers Zhu et al from the Harvard T.H. Chan School of Public Health and Massachusetts General Hospital analyzed data from 492,768 participants in the UK Biobank, which stores biologic samples from participants and is linked to their medical records. The researchers found 65,677 participants had asthma and 641 patients had severe COVID-19. “After adjusting for age, sex, body mass index, and other factors, the researchers found that having non-allergic asthma increased the risk of severe COVID-19 by as much as 48%. They also found that the risk of severe COVID-19 increased by as much as 82% among people with asthma and chronic obstructive pulmonary disease. Importantly, however, the study showed that people with allergic asthma had no statistically significant association with severe COVID-19.” The researchers published their results in the Journal of Allergy and Clinical Immunology in June.
Philanthropy’s Response to COVID-19 and Inequalities
Largest Cohort Study Yet Affirms No increased Mortality with COVID-19 in Asthma Patients
Posted July 20, 2020
On July 8, 2020, in the journal Nature, authors Elizabeth J. Williamson et al, reviewed results of the largest cohort study conducted by any country to date. They looked at risk factors connected to 10,926 COVID-19 deaths in the UK. They found that “COVID-19-related death was associated with: being male….; older age and deprivation (both with a strong gradient); diabetes; severe asthma; and various other medical conditions.” As explained by the COVID-19 Response Task Force of the American Academy of Allergy, Asthma, and Immunology, the study results suggested that asthma patients who had received oral steroids (OCS) in the past year also had increased mortality. They state, “However, when the data were limited to those in whom BMI, smoking history, and ethnicity were known (and, thus, could be controlled for), asthma with or without OCS use did not demonstrate a significant increased risk for death from COVID-19. Therefore, even with this paper, the preponderance of published data continues to demonstrate no increased severity or mortality with COVID-19 in asthma patients.”
Scientists Advocate for More Attention on the Role of Airborne Transmission of COVID-19
Posted July 13, 2020
On July 6th, authors Lidia Morawska and Donald K. Milton published, “It is Time to Address Airborne Transmission of COVID-19.“
Signed by 239 scientists, the stated purpose of the publication is: “We appeal to the medical community and to the relevant national and international bodies to recognize the potential for airborne spread of COVID-19. There is significant potential for inhalation exposure to viruses in microscopic respiratory droplets (microdroplets) at short to medium distances (up to several meters, or room scale), and we are advocating for the use of preventive measures to mitigate this route of airborne transmission.” The authors explain that multiple studies have demonstrated that viruses are released during exhalation, talking, and coughing in microdroplets small enough to remain aloft in air and pose a risk of exposure at distances beyond 1 to 2 m from an infected individual. This poses the risk that people sharing environments can potentially inhale these viruses, resulting in infection and disease. This problem is especially acute in indoor or enclosed environments, particularly those that are crowded and have inadequate ventilation relative to the number of occupants and extended exposure periods.
The authors recommend that, in addition to the current public health measures recommended, it is important to:
- Provide sufficient and effective ventilation (supply clean outdoor air, minimize recirculating air) particularly in public buildings, workplace environments, schools, hospitals, and aged care homes.
- Supplement general ventilation with airborne infection controls such as local exhaust, high efficiency air filtration, and germicidal ultraviolet lights.
- Avoid overcrowding, particularly in public transport and public buildings.
The main purpose of the publication was to ask the World Health Organization to acknowledge the role of aerosol transmission in the spread of COVID-19. Following this publication, the World Health Organization released a brief in which they maintain that the virus is mostly spread through close contact with infected people but call for more research into the matter of transmission by aerosolized particles.
While the relevance of this exchange is not directly tied to asthma, it has direct impacts on policies and practices related to indoor air quality, which do have a direct impact on asthma.
On July 1, 2020, the American Academy of Asthma Allergy and Immunology updated its information sheet on Caring for Pregnant Patients with Asthma During the COVID-19 Pandemic. The authors explain that “Few data exist to indicate that having asthma is associated with an increased risk of becoming infected with COVID-19 or a more severe course in the non-pregnant infected patient. Recent reassuring data show that having asthma was not associated with an increased risk of hospitalization or even mortality in COVID-19 hospitalized patients. There are even fewer data for pregnant asthmatic women with COVID-19.” Current recommendations emphasize the need to maintain asthma control during pregnancy. Reducing controller therapy could put pregnant women with asthma at increased risk of an asthma exacerbation necessitating medical care, which could then put them at an increased risk of being exposed to COVID-19. Questions addressed in this information sheet include:
- Is timing of delivery affected by COVID-19?
- Does COVID-19 present an increased risk of adverse perinatal and fetal outcomes?
- Is breastfeeding safe during COVID-19 infection?
- Are there ongoing studies to which pregnant women could be referred?
Posted June 29, 2020
A research letter published online in CHEST on June 6 by Lieberman-Cribbin W. et al noted that among the 11,405 patients within the Mount Sinai Health System in New York City who had a COVID-19 related hospital encounter, “asthma was not associated with a higher risk of mortality.” The authors also noted a low prevalence of asthma in the Mount Sinai Health System COVID-19 registry. The authors explain that there are limitations to their analysis: “asthma was self-reported, and information on treatments prior to admission, including inhaled or oral corticosteroids, was not available.” They suggest that further research is needed on the role of asthma and asthma medications in individual response to COVID-19.
Study Finds Neither a Diagnosis of Asthma nor Use of Inhaled Corticosteroids was Associated with an Increased Risk of COVID-19-related Hospitalization
Posted June 22, 2020
In a study published in the June 2020 edition of the Journal of Allergy and Clinical Immunology, authors Chibba et al assess the prevalence of asthma in hospitalized and non-hospitalized patients with COVID-19 through reviewing over 1,500 patient charts across 10 hospitals. Of 1,526 patients identified with COVID-19, 220 (14%) were classified as having asthma. Asthma was not associated with an increased risk of hospitalization after adjusting for age, sex, gender, and comorbidities. The ongoing use of inhaled coricosteroids did not increase the risk of hospitalization either. Anju T. Peters, MD, MSCI, FAAAAI, one of the study authors stated, “We would usually expect for asthmatic patients to have worse outcomes, as viral illness often can set off asthma exacerbations. More studies must be done to look at the underlying immune modulation caused by asthma or asthma treatment to see what impact it may have on COVID-19 outcomes.”
EPA Adds More Indoor Air Quality Questions and Answers to Its COVID-19 FAQ Webpage
Posted June 15, 2020
RAMP and partners working to reduce the burden of asthma have long recognized the importance of healthy indoor air quality. Whether we’re talking about improving air filtration and ventilation (through HVAC systems or portable air purifiers) or avoiding things that make the air quality worse (like environmental tobacco smoke or harmful cleaning products), we educate people about ways to reduce exposure to particulates and contaminants in the indoor air. But, as we’re in the midst of the COVID-19 pandemic, are there ways to reduce exposure to viruses as we address indoor air quality?
- Will an air cleaner or air purifier help protect me and my family from COVID-19 in my home?
- When used properly, air purifiers can help reduce airborne contaminants including viruses in a home or confined space. However, by itself, a portable air cleaner is not enough to protect people from COVID-19. When used along with other best practices recommended by the Centers for Disease Control and Prevention, operating an air cleaner can be part of a plan to protect yourself and your family.
- Can running the HVAC system in my home help protect me from COVID-19?
- By itself, running your HVAC system is not enough to protect yourself and your family from COVID-19. However, when used along with other best practices recommended by the Centers for Disease Control and Prevention, operating the HVAC system can be part of a plan to protect yourself and your family, since running your HVAC system filters the air as it is circulated.
- Where can professionals who manage school, office, and commercial buildings get information on ventilation and filtration to respond to COVID-19?
- Professionals who operate school, office, and commercial buildings should consult the American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) guidance for information on ventilation and filtration to help reduce risks from the virus that causes COVID-19. In general, increasing ventilation and filtration is usually appropriate; however, due to the complexity and diversity of buildings types, sizes, construction styles, HVAC system components, and other building features, a professional should interpret ASHRAE guidelines for their specific building and circumstances.
CDC and AAAAI Differ on Asthma Management at School During COVID-19 Pandemic
Posted June 8, 2020
On June 3, 2020, the US Centers for Disease Control and Prevention updated their FAQs on students returning to school in the context of the COVID-19 pandemic. Specifically related to students with asthma, the FAQs address: asthma treatments with inhalers/spacers, the use of nebulizers, and the use of peak flow meters.
- Asthma treatments using inhalers with spacers are preferred over nebulizer treatments whenever possible.
- Nebulizer treatments at school should be reserved for children who cannot use or do not have access to an inhaler
- Peak flow meters can be used in schools
- Schools should obtain the appropriate personal protective equipment (PPE) for staff who administer nebulizer treatments and peak flow meters to students with asthma.
More detail, including the studies cited by the CDC in the development of their recommendations can be found here.
- The CDC suggests that aerosols generated from nebulizers may not be infectious. The task force states, “The supporting data for this is very poor, however.”
- The task force does not believe the CDC goes far enough with their PPE recommendations for performing nebulized therapy
- The task force questions the overall safety of peak flow usage in public without wearing gloves, mask and eye coverage.
The AAAAI response can be found here (scroll toward the bottom of the page for the relevant post).
Asthma, Spirometry and COVID-19
Posted June 1, 2020
In late May, 2020, two articles were published on the use of lung function testing during the COVID-19 pandemic. On May 29th, the Lancet published “Lung function testing in the COVID-19 endemic” by James H Hull et al. On May 24th, the Italian Journal of Pediatrics published “Italian Pediatric Respiratory Society Recommendations on Pediatric Pulmonary Function Testing During COVID-19 Pandemic” by Elisabetta Bignamini et al. The Lancet authors, in reference to spirometry, state, “This procedure requires patients to repeatedly undertake forced exhalatory manoeuvres and as such frequently precipitates coughing and the production of sputum. It also requires clinicians and patients to be in close proximity and thus, even with the use of device filters, in a COVID endemic phase, enhanced infection prevention and control is crucial.” Recognizing this concern, the Italian Journal of Pediatrics authors state, “Pulmonary function testing should be performed in children with chronic lung disease only if it is needed to guide management.” While spirometry is a key component of asthma diagnosis and management, the concerns expressed in these articles mirror statements from the American Academy of Allergy, Asthma, and Immunology (AAAAI) and the American Thoracic Society. The AAAAI statement includes, “As things begin to open up there will be pressure to resume spirometry and ENO, but these will all require the use of full PPE (face mask, N95 respirator, gown, and gloves)…. As PPE becomes more available, spirometry and ENO could then be resumed in outpatient offices — provided full PPE is used, as per the CDC guidelines.”
New data on COVID-19 mortality by race and ethnicity underscore disparities
Posted on May 26th, 2020
New figures compiled by the non-partisan APM Research Lab and released on May 20th provide further evidence of the staggering divide in the COVID-19 death rate between black Americans and the rest of the United States population. Authors were able to gather and analyze data on race and ethnicity for 88% of COVID-19 deaths across 40 states and the District of Columbia. Of note, 1 in 2,000 Black Americans has died (or 50.3 per 100,000), at a rate 2.4 times higher than whites. The authors describe other racial disparities, explaining “If they had died of COVID-19 at the same rate as White Americans, about 12,000 Black Americans, 1,300 Latino Americans and 300 Asian Americans would still be alive.” Click here to view the full report, titled, The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S.
Impact of asthma medications on COVID outcomes
Posted on May 11th, 2020
On May 6, 2020, in the Annals of Allergy, Asthma & Immunology, Johns Hopkins researchers published “Asthma, Biologics, Corticosteroids, and COVID-19.” The authors reinforce the message that current data on the risk of acquiring COVID-19 or disease severity in patients with asthma is limited and they identify recommendations for future research (in the table below). In this article, they share information about the impact on COVID-19 of both steroids and biologics used to treat asthma. The researchers believe that the effect of steroids on acquiring COVID-19 and/or the severity of COVID-19 likely depends on a number of individual factors, including baseline asthma control and dose of the steroid. They do not believe any of the biologics used for asthma treatment would increase the risk of acquiring COVID-19 or the severity of it. They state, “On the contrary, we postulate that the reversal of the Th2 skew and the improvement in airway allergic and eosinophilic inflammation and bronchial responsiveness induced by these biologics, could be advantageous in patients with asthma who are already on these medications prior to contracting COVID-19.” They conclude that, as we continue to learn more, patients with asthma should continue to exercise caution to prevent contracting the disease.
For a full sized version of the table, click on the image.

Obesity may lead to more severe COVID outcomes among younger individuals
Posted on May 4th, 2020
On April 30, 2020, researchers from Johns Hopkins University published “Obesity could shift severe COVID-19 disease to younger ages“ in The Lancet. The researchers looked at obesity as a potential factor influencing the younger age of people admitted to the ICU in the United States, as compared to China, Spain, and Italy. They noted that prevalence of obesity in the United States is around 40%, versus a prevalence of 6.2% in China, 20% in Italy, and 24% in Spain. The researchers found a significant inverse correlation between age and body mass index, in which younger individuals admitted to the hospital were more likely to be obese “Obesity can restrict ventilation by impeding diaphragm excursion, impairs immune responses to viral infection, is pro-inflammatory, and induces diabetes and oxidant stress to adversely affect cardiovascular function. We conclude that in populations with a high prevalence of obesity, COVID-19 will affect younger populations more than previously reported. Public messaging to younger adults, reducing the threshold for virus testing in obese individuals, and maintaining greater vigilance for this at-risk population should reduce the prevalence of severe COVID-19 disease.” This is important information for asthma stakeholders as obesity is significantly associated with the development of asthma, worsening asthma symptoms, and poor asthma control.
Data on the risk of severe COVID among people with asthma
Posted on April 27th, 2020
On April 23rd, the Editorial Team from The Lancet Respiratory Medicine published, Reflecting on World Asthma Day in the era of COVID-19. They note that there has been debate about the risk of severe COVID among people with asthma, stating, “It was predicted that patients with chronic respiratory diseases would be more vulnerable both to infection and to subsequent severe disease.” However, that presumption does not align with medical literature to date. In fact, the previous day, April 22nd, the Journal of the American Medical Association published, Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area by Richardson et al, showing that just 9% of people hospitalized in New York due to COVID had asthma (which is lower than state asthma prevalence.) The Lancet Editorial Team speculates that lower reported prevalence across several studies, “might be due to underdiagnosis or lack of recognition of chronic respiratory diseases in those with COVID-19, effects of differing immune responses elicited by chronic respiratory diseases, or a protective effect of inhaled corticosteroids.”
Impacts of smoking and COPD on COVID outcomes
Posted on April 23rd, 2020
Last week, on April 15th, researchers from China published an article in the Journal of Medical Virology looking at the impact of COPD and smoking on the development of severe COVID-19. They conducted a meta-analysis and found that COPD increased the likelihood of severe COVID-19 outcomes by 4.38, while smoking increased the likelihood of severe outcomes by 1.98. Similarly, researchers at UCSF also conducted a meta-analysis and shared in a pre-print version of their article that they found a 2.25 odds ratio of progression of COVID-19 among smokers. These studies underscore the importance of helping people quit smoking. For those in California, the California Smokers’ Helpline remains available during the pandemic online at https://info.nobutts.org/ or at 1-800-NO-BUTTS.

